vintage weaver k4
There have been several efforts to assist the analysis of the NST by the application of computerized systems. Related Topics Bird Animal Nature Outdoors and Nature comments sorted by Best Top New Controversial Q&A Add a Comment More posts you may like. Factors influencing generation of FHR pattern. The presence of a saltatory pattern, especially when paired with decelerations, should warn the physician to look for and try to correct possible causes of acute hypoxia and to be alert for signs that the hypoxia is progressing to acidosis.21 Although it is a nonreassuring pattern, the saltatory pattern is usually not an indication for immediate delivery.19. Per the ACOG Coding Committee, the following is a brief description of CPT code 59025, Fetal NST: "The patient reports fetal movement as an external monitor records fetal heart rate changes. Obstet Gynecol Surv 41: 121, 1986, Dalton KJ, Dawes GS, Patrick JE: The autonomic nervous system and fetal heart rate variability. WebThe biophysical profile is a test used to evaluate the well-being of the fetus. Preliminary studies have compared the output of the System 8000 to conventional NST assessment.63, 64 These independent investigations concluded that such systems, designed to be consistent and objective, could serve in primary screening when experts are not immediately available. The testing protocol used at the Medical College of Georgia is outlined in Table 1. Am J Obstet Gynecol 142: 363, 1982, Gelman SR, Spellacy WN, Wood S et al: Fetal movements and ultrasound: Effect of maternal intravenous glucose administration. You may see, Establishing Paternity with Paternity Tests, Can I get pregnant ifand other questions about conception, Products & Tests to Support Your Pregnancy, Supplements and Medications for a Healthy Pregnancy, You sense the baby is not moving as frequently as usual, There is any reason to suspect the placenta is not functioning adequately. Am J Obstet Gynecol 148: 35, 1984, Martin CB: Behavioral states in the human fetus. Accessed Dec. 5, 2022. Am J Obstet Gynecol 134: 460, 1979, Leveno KJ, Williams ML, DePalma RT et al: Perinatal outcome in the absence of antepartum fetal heart rate acceleration. 2. Prematurity, It indicates severe fetal anemia, as occurs in cases of Rh disease or severe hypoxia.24 It should be differentiated from the pseudosinusoidal pattern (Figure 11a), which is a benign, uniform long-term variability pattern. American College of Obstetricians and Gynecologists. Fetal bradycardia is defined as a baseline heart rate less than 120 bpm. Nonrandom, periodic cycles of FHR are generated, lasting from 60 to 500 minutes,16 with a mean duration of approximately 90 minutes at term. WebThe normal FHR range is between 120 and 160 beats per minute (bpm). The monitor calculates and records the FHR on a continuous strip of paper. Document in detail interpretation of FHR, clinical conclusion and plan of management. (Before 28 weeks, the test isn't accurate.) External tokodynamometer devices are used to register uterine activity. Pros cons. Developments in the areas of automated analysis, actocardiography, and objective clinical archives should lead to improved and more appropriate use of FHR testing. The NST has become useful in antenatal surveillance because of wide applicability, ease of performance, and relatively low cost.75 Its ability to produce rapid results enables testing centers to screen high volumes of at-risk pregnancies efficiently. Obstet Gynecol 82: 999, 1993, Devoe L, Boehm F, Paul R et al: Clinical experience with the Hewlett Packard M-1350 fetal monitor: Correlation of doppler-detected fetal body movements with fetal heart rate parameters and perinatal outcome. Br J Obstet Gynaecol 89: 716, 1982, Flynn AM, Kelly J, Mansfield H et al: A randomized controlled trial of nonstress antepartum cardiotocography. Am J Obstet Gynecol 141: 646, 1981, Devoe LD, McKenzie J, Searle NS et al: Clinical sequelae of the extended nonstress test. In one study,37 the incidence of pathologic CSTs following prolonged nonreactivity was 93%, implying that the absence of accelerations for 90 minutes or more in nonanomalous term fetuses is itself a strong sign of fetal compromise. These pathways are evident as early as the midtrimester.6 FHR decelerative responses are partly generated through parasympathetic pathways, resulting from direct vagal stimulation and baroreceptor and chemoreceptor arcs (aortic arch, carotid sinus).9. Some clinicians have argued that this unproven technology has become the standard for all patients designated high risk and has been widely applied to low-risk patients as well.9 The worldwide acceptance of EFM reflects a confidence in the importance of electronic monitoring and concerns about the applicability of auscultation.10 However, in a 1996 report, the U.S. Preventive Services Task Force7 did not recommend the use of routine EFM in low-risk women in labor. Webby selecting a one minute segment of trace, without accelerations or decelerations and measuring the difference between the highest and lowest rate. Clinically, loss of beat-to-beat variability is more significant than loss of long-term variability and may be ominous.18 Decreased or absent variability should generally be confirmed by fetal scalp electrode monitoring when possible. U.S. STD Cases Increased During COVIDs 2nd Year, Pesticide in Produce: See the Latest Dirty Dozen, Having A-Fib Might Raise Odds for Dementia, New Book: Take Control of Your Heart Disease Risk, MINOCA: The Heart Attack You Didnt See Coming, Health News and Information, Delivered to Your Inbox, Pregnant With Allergies? Am J Obstet Gynecol 133: 579, 1979, Keegan KA, Paul RH, Broussard PM et al: Antepartum fetal heart rate testing: III. Therefore, interpretation of the NST may be generalized to include the occurrence of at least one FHR acceleration with movement during the baseline period,68 a normal baseline FHR,69 the absence of periodic or spontaneous FHR decelerations,70 and, in some schemes, the presence of normal baseline variability.71, 72, 73 An NST may be nonreactive if accelerations are absent or subnormal in their dimensions (amplitude, duration) and fetal movements are absent or do not elicit FHR accelerations. Regardless of the depth of the deceleration, all late decelerations are considered potentially ominous. Br J Obstet Gynecol 99: 685, 1992, Maeda K: Studies on new ultrasonic doppler fetal actograph and continuous recordings of fetal movement. Total test time >5. Nevertheless, the tendency of these systems to exaggerate baseline variability through artifactual jitter has been greatly reduced.41 A tracing with minimal or absent baseline fluctuations is cause for some concern, regardless of the instrumentation used to capture the FHR signal. WebHealthy babies will respond with an increased heart rate during times of movement, and the heart rate will decrease at rest. Movement, heart rate and reactivity of heart rate to movement are measured for 20-30 minutes. WebThe Difference Between Hospital Emergency Rooms and Urgent Care Centers Both urgent care centers and emergency rooms provide patients with medical care, but these two facilities are not designed or equipped to handle the same situations. A normal nonstress test will show a baseline fetal heart rate between 110 and 160 beats per minute with moderate variability (5- to 25-interbeat variability) and 2 qualifying accelerations in 20 minutes with no decelerations. Am J Obstet Gynecol 155: 10, 1986, Brown V, Sawers RS, Parsons RJ et al: The value of antenatal cardiotocography in the management of high risk pregnancy: A randomized controlled trial. There are five components measured during the biophysical examination. The fetal heart rate (FHR) pattern can be analyzed visually by describing the However, absolute and relative contraindications to the CST have been established. Am J Obstet Gynecol 130: 765, 1978, Lyons ER, Bylsma-Howell M, Siamsi S et al: A scoring system for nonstressed antepartum fetal heart rate monitoring. Such approaches were intended to assist high risk care but not to substitute for contextual evaluation using all available data. The nonstress test as a primary approach. A regular ultrasound uses sound waves to produce images, but can't show blood flow. However, the inability of the placenta to exchange oxygen and carbon dioxide results in fetal respiratory acidosis. Get prescriptions or refills through a video chat, if the doctor feels the prescriptions are medically appropriate. Over 20,000 resources for health professionals, The Alliance for Fig. Your due date has passed. The FHR recordings may be interpreted as reassuring, nonreassuring or ominous, according to the pattern of the tracing. While the CST remains a very robust test of placental well-being, its logistic constraints and time requirements have led toits gradual replacement by either complete BPP testing (all five components) or modified BPP testing (NST and amniotic fluid volume assessment). Results in this range must also be interpreted in light of the FHR pattern and the progress of labor, and generally should be repeated after 15 to 30 minutes. Earlier approaches had advocated manual palpation or shaking of the fetal head or body. Am J Obstet Gynecol 144: 574, 1982, Bourgeois FJ, Thiagarajah S, Harbert GM: The significance of fetal heart rate decelerations during nonstress testing. WebAbstract. Absence of reactive accelerations. Grade 2: The cells and tissue are somewhat abnormal and are called moderately differentiated. In Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP (eds): Cochrane Database of Systematic Reviews. The corollary to this situation would be marked decreases in acceleration frequency. Practical considerations dictate that the NST not be used prior to the age at which neonatal survival is possible. Postdate gestation, preeclampsia, chronic hypertension and diabetes mellitus are among the causes of placental dysfunction. CTG is used both before birth While considerable time has been expended on the development and description of these systems, sufficient trials of clinical efficacy are yet to be undertaken. Hi doctors, is HIV Alere Combo negative test conclusive at week 11 (85 days)? Am J Obstet Gynecol 130: 232, 1978, Evertson LR, Gauthier RJ, Collea JV: Fetal demise following negative contraction stress tests. 12th ed. 7. Obstet Gynecol 63: 528, 1984, Nayot D, Mor-YoSef S, Granat M et al: Antepartum fetal heart rate pattern associated with major congenital malformations. Overall, the use of primary nonstress testing with selective CSTs has been shown to be an effective means of economizing testing efforts without reducing the diagnostic potential of FHR testing. More recently, Devoe and co-workers,122 reported a prospective collaborative study comparing the NST and nipple stimulation CST in 1270 patients. It should be carefully noted that other mechanisms may be responsible for late FHR decelerations: (1) intrinsic maternal hypoxemia (respiratory disease, anemia); (2) maternal hypotension (aortocaval compression, drugs); or (3) compromise of umbilical venous blood flow (partial cord occlusion). Table 1. 2005 - 2023 WebMD LLC, an Internet Brands company. The presence of at least two accelerations, each lasting for 15 or more seconds above baseline and peaking at 15 or more bpm, in a 20-minute period is considered a reactive NST. Grades of fluctuation are based on amplitude range (peak to trough): Absent variability = Amplitude range undetectable Minimal = < 5 BPM Moderate = 6 to 25 BPM Marked = > 25 BPM
2021; doi: 10.1097/AOG.0000000000004407. The test can indicate if the baby is not receiving enough oxygen because of placental or umbilical cord problems; it can also indicate other types of fetal distress. Usually, a baby's heart beats faster during activity. Finally, the quality of recorded signals is a limiting factor for interpretation. 5. While a nonstress test can bring relief about your baby's health, it may cause worry too. Lippincott Williams & Williams, 2010. Am J Obstet Gynecol 134: 36, 1979, Hammacher K: The clinical significance of cardiotocography. Review no. Although these decelerations are not associated with fetal distress and thus are reassuring, they must be carefully differentiated from the other, nonreassuring decelerations. Obstet Gynecol 45: 433, 1975, Trimbos JB, Keirse MJNC: Significance of antepartum cardiotocography in normal pregnancy. Practice Bulletin No. This will ensure that the CTG is saved to the correct electronic record. It also helps make sure your test results are correct. The baseline rate is interpreted as changed if the alteration persists for more than 15 minutes. Healthy babies will respond with an increased heart rate during times of movement, and the heart rate will decrease at rest. Range 30-100 ng/ml. DeCherney AH, et al., eds. 03881, March 24, 1993. 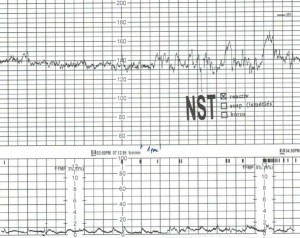 Other maternal conditions such as acidosis and hypovolemia associated with diabetic ketoacidosis may lead to a decrease in uterine blood flow, late decelerations and decreased baseline variability.23. Am J Obstet Gynecol 147: 451, 1983, Natale R, Nasello-Patterson C, Turok R: Longitudinal measurements of fetal breathing, body movements, heart rate, and heart rate accelerations and decelerations at 24 to 32 weeks of gestation. McGraw Hill; 2019. https://accessmedicine.mhmedical.com/search. In: Perinatal Factors Affecting Human Development, p 96. WebThe NST (with or without amniotic fluid assessment) has become the preferred antepartum test of fetal oxygenation status because the CST, which usually requires Regardless of FHR responses during hyperstimulation, a rest period of at least 12 hours is recommended if further contraction stress testing is to be performed. The test might show a need for further care or testing. Obstet Gynecol 51: 614, 1978. Reactivity in preterm fetuses may be characterized by a higher incidence of low amplitude (1015 beats/min) accelerations,10 weaker coupling between fetal movements and accelerations,11 and more frequent mild decelerations.10 Devoe and Azor demonstrated that simultaneous nonstress testing of twin pregnancy was feasible with a high rate of legible recordings.82 Rh sensitization presents a relatively unique antenatal problem for FHR testing in that fetal problems include reduced oxygen-carrying capacity, umbilical cord compression secondary to hepatomegaly, and intravascular volume disturbances. Extending the length of the initial NST36, 37 for as long as 120 minutes may be useful in improving the classification of normal and abnormal fetuses. Many people do not know the difference between the two methods or why one might be selected over the other. Sinusoidal Pattern: A regular, smooth, undulating signal, resembling a sine wave, with an amplitude of 5-15bpm, and a frequency cycle Best time for a conference call or a meeting is between 4pm-6pm in GMT which corresponds to 8am-10am in PST. Unfortunately, precise information about the frequency of false-positive results is lacking, and this lack is due in large part to the absence of accepted definitions of fetal distress.7 Meta-analysis of all published randomized trials has shown that EFM is associated with increased rates of surgical intervention resulting in increased costs.8 These results show that 38 extra cesarean deliveries and 30 extra forceps operations are performed per 1,000 births with continuous EFM versus intermittent auscultation. Disk Issue 1. Normative data for simultaneous twin NSTs show synchrony or similarity in the tracings with incidences of 57.14% and 58% in twins monitored from 27 weeks until term ( Devoe and Azor, 1981 ; Sherer et al., 1990 ). WebNo distinction is made between short-term variability (or beat-to-beat variability or R-R wave period differences in the electrocardiogram) and long-term variability. Doctors typically provide answers within 24 hours. Given the limitations of arbitrary interpretative criteria, based on cutoff points or past clinical experience, such errors are inevitable. A positive CST (Fig. It may also be performed using an external transducer, which is placed on the maternal abdomen and held in place by an elastic belt or girdle. Prematurity decreases variability16; therefore, there is little rate fluctuation before 28 weeks. 2021; doi:10.1097/AOG.0000000000004411. The NST is an effective approach for evaluating a wide range of potential antenatal problems, including intrauterine growth retardation (IUGR),76, 77 prolonged gestation,78, 79 preterm pregnancy,38, 80 multiple gestation,81, 82, 83 Rh sensitization,35 and anomalies.84, 85. These include the optimal timing of test initiation, post-test risk adjustment for specific high risk conditions, and testing of fetuses between 24 and 32 weeks' gestation. Washington, DC, Pan American Health Organization, 1969, Kubli FW, Kaeser O, Hinselmann M: Diagnostic management of chronic placental insufficiency. In this case, non-stress testing may start as early as.
Other maternal conditions such as acidosis and hypovolemia associated with diabetic ketoacidosis may lead to a decrease in uterine blood flow, late decelerations and decreased baseline variability.23. Am J Obstet Gynecol 147: 451, 1983, Natale R, Nasello-Patterson C, Turok R: Longitudinal measurements of fetal breathing, body movements, heart rate, and heart rate accelerations and decelerations at 24 to 32 weeks of gestation. McGraw Hill; 2019. https://accessmedicine.mhmedical.com/search. In: Perinatal Factors Affecting Human Development, p 96. WebThe NST (with or without amniotic fluid assessment) has become the preferred antepartum test of fetal oxygenation status because the CST, which usually requires Regardless of FHR responses during hyperstimulation, a rest period of at least 12 hours is recommended if further contraction stress testing is to be performed. The test might show a need for further care or testing. Obstet Gynecol 51: 614, 1978. Reactivity in preterm fetuses may be characterized by a higher incidence of low amplitude (1015 beats/min) accelerations,10 weaker coupling between fetal movements and accelerations,11 and more frequent mild decelerations.10 Devoe and Azor demonstrated that simultaneous nonstress testing of twin pregnancy was feasible with a high rate of legible recordings.82 Rh sensitization presents a relatively unique antenatal problem for FHR testing in that fetal problems include reduced oxygen-carrying capacity, umbilical cord compression secondary to hepatomegaly, and intravascular volume disturbances. Extending the length of the initial NST36, 37 for as long as 120 minutes may be useful in improving the classification of normal and abnormal fetuses. Many people do not know the difference between the two methods or why one might be selected over the other. Sinusoidal Pattern: A regular, smooth, undulating signal, resembling a sine wave, with an amplitude of 5-15bpm, and a frequency cycle Best time for a conference call or a meeting is between 4pm-6pm in GMT which corresponds to 8am-10am in PST. Unfortunately, precise information about the frequency of false-positive results is lacking, and this lack is due in large part to the absence of accepted definitions of fetal distress.7 Meta-analysis of all published randomized trials has shown that EFM is associated with increased rates of surgical intervention resulting in increased costs.8 These results show that 38 extra cesarean deliveries and 30 extra forceps operations are performed per 1,000 births with continuous EFM versus intermittent auscultation. Disk Issue 1. Normative data for simultaneous twin NSTs show synchrony or similarity in the tracings with incidences of 57.14% and 58% in twins monitored from 27 weeks until term ( Devoe and Azor, 1981 ; Sherer et al., 1990 ). WebNo distinction is made between short-term variability (or beat-to-beat variability or R-R wave period differences in the electrocardiogram) and long-term variability. Doctors typically provide answers within 24 hours. Given the limitations of arbitrary interpretative criteria, based on cutoff points or past clinical experience, such errors are inevitable. A positive CST (Fig. It may also be performed using an external transducer, which is placed on the maternal abdomen and held in place by an elastic belt or girdle. Prematurity decreases variability16; therefore, there is little rate fluctuation before 28 weeks. 2021; doi:10.1097/AOG.0000000000004411. The NST is an effective approach for evaluating a wide range of potential antenatal problems, including intrauterine growth retardation (IUGR),76, 77 prolonged gestation,78, 79 preterm pregnancy,38, 80 multiple gestation,81, 82, 83 Rh sensitization,35 and anomalies.84, 85. These include the optimal timing of test initiation, post-test risk adjustment for specific high risk conditions, and testing of fetuses between 24 and 32 weeks' gestation. Washington, DC, Pan American Health Organization, 1969, Kubli FW, Kaeser O, Hinselmann M: Diagnostic management of chronic placental insufficiency. In this case, non-stress testing may start as early as.  Most testing schemes use a fixed threshold for a minimum frequency of FHR accelerations in a given length of observation. Studies of interobserver and intraobserver differences in the evaluation of FHR tests have isolated two key problems associated with their visual interpretations: inconsistency in evaluating pathologic tracings out of context,125 and decreased consistency among observers as the number of diagnostic categories is increased.126 Inadequate length of observation, failure to account for different standards related to gestational age, and nonstandardization of maternal status (e.g., drug administration, activity levels, and so on) may also confuse interpretation of subsequent FHR test patterns. This content is owned by the AAFP. Subsequent reports of fetal death during this intervening period115, 116, 117, 118 must be considered as rare failures of detection, since the majority were due to unanticipated obstetric accidents. Regardless of specific interpretative criteria, several considerations are important for proper utilization of the NST: (1) gestational age at test initiation, (2) frequency of test repetition, and (3) mode of test follow-up. During the nonstress test, you'll lie on a reclining chair. Long-term variability is a somewhat slower oscillation in heart rate and has a frequency of three to 10 cycles per minute and an amplitude of 10 to 25 bpm. WebThese are called well-differentiated tumors and are considered low grade. NST is the test CTG is the recording of the test. Umana OD, et al. An intravenous line is then started with normal saline and oxytocin infusion begun through an auxiliary or piggyback line at an initial rate of 0.5 mU per minute. We use cookies to ensure you get the best experience from our website.By using the website or clicking OK we will assume you are happy to receive all cookies from us. Table 3 lists examples of nonreassuring and ominous patterns. sleep patterns, certain maternal prescription or nonprescription drugs). Imaging of the different molecular subtypes has revealed that biologically different tumors often exhibit typical features in mammography, ultrasound, and MRI. Pitfalls in the applications of the FHR tests may also reflect differences among observers, differing interpretative criteria, uncontrolled testing conditions, characteristics of the electronic monitoring equipment used, and inappropriate clinical responses to test outcomes. Your baby's heart should beat faster when active -- just like yours. Recently, second-generation fetal monitors have incorporated microprocessors and mathematic procedures to improve the FHR signal and the accuracy of the recording.3 Internal monitoring is performed by attaching a screw-type electrode to the fetal scalp with a connection to an FHR monitor. Identify changes in the FHR recording over time, if possible. Under normal conditions, the placenta serves as a respiratory and nutritive organ. Interpretation of the FHR variability from an external tracing appears to be more reliable when a second-generation fetal monitor is used than when a first-generation monitor is used.3 Loss of variability may be uncomplicated and may be the result of fetal quiescence (rest-activity cycle or behavior state), in which case the variability usually increases spontaneously within 30 to 40 minutes.19 Uncomplicated loss of variability may also be caused by central nervous system depressants such as morphine, diazepam (Valium) and magnesium sulfate; parasympatholytic agents such as atropine and hydroxyzine (Atarax); and centrally acting adrenergic agents such as methyldopa (Aldomet), in clinical dosages.19. Cardiotocography (CTG) is the current standard of care for external monitoring of a fetus during a non-stress test (NST) and a contraction stress test (CST), as well as during labor. Retrospective studies of the NST by Platt and associates134 and of the CST by Garite and colleagues135 indicate that the use of FHR testing has been linked to a significant reduction in antepartum fetal deaths. Differentiating between a reassuring and nonreassuring fetal heart rate pattern is the essence of accurate interpretation, which is essential to guide appropriate triage decisions. Best time for a conference call or a meeting is between 4pm-6pm in GMT which corresponds to 8am-10am in PST. In: StatPearls. A cardiotocography is a technique that is used to monitor the heartbeat of the foetus along with keeping a check on uterine contractions. WebTime conversion from Greenwich Mean Time (+0) to Pacific Standard Time(-8) to EET (Eastern European Time)(+2) to Newfoundland Standard Time(-3) to Alaska Daylight Time(-8) to PDT (Pacific Daylight Time)(-7) to Central Standard Time(-6) to Eastern Standard Time(-5). Mosby: 2010. Fetal heart rate patterns are classified as reassuring, nonreassuring or ominous. bed on the whiteboard. Common examples of risk include prolonged pregnancy; maternal hypertensive disorders; intrauterine growth retardation; diabetes mellitus; Rh sensitization; maternal hemoglobinopathies; renal disease; cardiac disease; fetal anomalies; poor prior obstetric history; and reported decrease in perceived fetal movement. The incidence of reactive tests associated with subsequently negative CSTs is nearly 100%. The concept behind a non-stress test is that adequate oxygen is required for fetal activity and heart rate to be within normal ranges. This requires frequent palpation of the uterine fundus and accurate placement of the tokodynamometer. These states of active sleep occupy 4060% of the average 24-hour day18 and are also reflected by increased baseline FHR variability. The test involves attaching one belt to the mothers abdomen to measure fetal heart rate and another belt to measure contractions. If your baby doesn't move during the NST, try not to worry. Note association of accelerations with fetal movements. It is also important to remember that interpretative standards different from those used at term should be applied to these earlier gestational ages. To date, there have been four randomized controlled clinical trials of NST as a primary screening method for high risk pregnancy.128, 129, 130, 131 While most current practices would perform testing more frequently than was the case in these trials (at least twice weekly as opposed to once weekly), it is interesting to note that NSTs were generally not the only well-being tools used. Web2. Br J Obstet Gynaecol 87: 270, 1980, Vorher H: Placental insufficiency in relation to post-term pregnancy and fetal postmaturity. Why is the doctor wanting me to do a blood test, saying it might show a difference in my allergy levels. The stimulator is applied to the maternal abdomen in the region of the fetal head, then a 3-second pulse is delivered. A single copy of these materials may be reprinted for noncommercial personal use only. They are usually associated with fetal movement, vaginal examinations, uterine contractions, umbilical vein compression, fetal scalp stimulation or even external acoustic stimulation.15 The presence of accelerations is considered a reassuring sign of fetal well-being. Under adverse circumstances (e.g., decreased utero-placental perfusion or maternal malnutrition), these stores may be prematurely exhausted; consequently, fetal growth and energy-dependent biophysical activities are curtailed. In a large longitudinal study of fetuses who exhibited a combination of nonreactivity, reduced variability, and spontaneous decelerations, Beischer and associates124 found that 93% of surviving infants available for follow-up had no major neurologic handicap. Am J Obstet Gynecol 133: 685, 1979, Peeters LL, Shelton RE, Jones MD et al: Blood flow to fetal organs as a function of arterial oxygen content. Br J Obstet Gynaecol 89: 427, 1982, Kidd LC, Patel NB, Smith R: Nonstress antenatal cardiotocographya prospective randomized clinical trial. Most obstetric laboratories now use FHR transducers operating in either continuous or pulsed Doppler modes rather than phonocardiographic or abdominal electrocardiographic signal sources. Am J Obstet Gynecol 135: 1071, 1979, Nathanielsz PW, Bailey A, Poore ER et al: The relationship between myometrial activity and sleep state and breathing in fetal sheep throughout the last third of gestation. This is presumptive support of the effectiveness of the reactive test alone in identifying uncompromised fetuses. In the absence of acidosis, acute disturbances of placental respiratory or nutritive function may result in sudden and profound decrease in fetal movement incidence. WebLow risk patients with metastatic disease were, however, significantly more likely to need to change to second line chemotherapy than patients with non-metastatic GTN although Am J Obstet Gynecol 170: 650, 1994, Searle JR, Devoe LD, Phillips MC, Searle NS: Computerized analysis of resting fetal heart rate tracings. In Pecile A, Finzi C (eds): The Foeto-Placental Unit, p 323. Br J Obstet Gynaecol 84: 39, 1977, Schifrin BS, Lapidus M, Doctor GS et al: Contraction stress for antepartum fetal evaluation. Fetal tachycardia may be a sign of increased fetal stress when it persists for 10 minutes or longer, but it is usually not associated with severe fetal distress unless decreased variability or another abnormality is present.4,11,17. Labour and delivery: all you need to know, Pregnancy diet plans: trimester by trimester, Pregnancy symptoms you should never ignore, , : , : , : . It is important to maintain proper perspective on the place of FHR testing in overall clinical management. Am J Obstet Gynecol 151: 1074, 1985, Devoe LD: Antepartum fetal heart rate testing in pre-term pregnancy. Mayo Clinic on Incontinence - Mayo Clinic Press, NEW Mayo Clinic on High Blood Pressure - Mayo Clinic Press, Mayo Clinic on Hearing and Balance - Mayo Clinic Press, FREE Mayo Clinic Diet Assessment - Mayo Clinic Press, Mayo Clinic Health Letter - FREE book - Mayo Clinic Press, Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic School of Continuous Professional Development, Mayo Clinic School of Graduate Medical Education, Book: Mayo Clinic Guide to a Healthy Pregnancy. This content does not have an English version. Talk to your health care provider about your nonstress test results. This finding during the CST should prompt ultrasound examination for amniotic fluid volume, or umbilical cord localization. New York, Academic Press, 1970, Lee CY, Diloreto PC, O'Lane JM: A study of fetal heart rate acceleration patterns. GMT to Kaliningrad call time. If the results are unusual, your doctor may suggest further testing. Of the various FHR testing schemes that have been studied, two primary methods for Table 4 lists recommended emergency interventions for nonreassuring patterns.4,14 These interventions should also be considered for ominous patterns while preparations for immediate delivery are initiated. 9. You can get one of two results from an NST: Reactive: This result means that your babys heart rate went up to the expected level at least twice during the test. Those with a reactive baseline are at much lower risk for intrauterine or neonatal compromise, while those with nonreactive CSTs constitute the highest risk group within the populations studied to date.91, 92, 93, 94 It is probable that a number of false positive tests occur in the former subgroup, and, as suggested by Devoe,103 only 10% developed evidence of intrapartum fetal distress when vaginal delivery was attempted. The most significant factor that influences fetal response to VAS appears to be gestational age.
Most testing schemes use a fixed threshold for a minimum frequency of FHR accelerations in a given length of observation. Studies of interobserver and intraobserver differences in the evaluation of FHR tests have isolated two key problems associated with their visual interpretations: inconsistency in evaluating pathologic tracings out of context,125 and decreased consistency among observers as the number of diagnostic categories is increased.126 Inadequate length of observation, failure to account for different standards related to gestational age, and nonstandardization of maternal status (e.g., drug administration, activity levels, and so on) may also confuse interpretation of subsequent FHR test patterns. This content is owned by the AAFP. Subsequent reports of fetal death during this intervening period115, 116, 117, 118 must be considered as rare failures of detection, since the majority were due to unanticipated obstetric accidents. Regardless of specific interpretative criteria, several considerations are important for proper utilization of the NST: (1) gestational age at test initiation, (2) frequency of test repetition, and (3) mode of test follow-up. During the nonstress test, you'll lie on a reclining chair. Long-term variability is a somewhat slower oscillation in heart rate and has a frequency of three to 10 cycles per minute and an amplitude of 10 to 25 bpm. WebThese are called well-differentiated tumors and are considered low grade. NST is the test CTG is the recording of the test. Umana OD, et al. An intravenous line is then started with normal saline and oxytocin infusion begun through an auxiliary or piggyback line at an initial rate of 0.5 mU per minute. We use cookies to ensure you get the best experience from our website.By using the website or clicking OK we will assume you are happy to receive all cookies from us. Table 3 lists examples of nonreassuring and ominous patterns. sleep patterns, certain maternal prescription or nonprescription drugs). Imaging of the different molecular subtypes has revealed that biologically different tumors often exhibit typical features in mammography, ultrasound, and MRI. Pitfalls in the applications of the FHR tests may also reflect differences among observers, differing interpretative criteria, uncontrolled testing conditions, characteristics of the electronic monitoring equipment used, and inappropriate clinical responses to test outcomes. Your baby's heart should beat faster when active -- just like yours. Recently, second-generation fetal monitors have incorporated microprocessors and mathematic procedures to improve the FHR signal and the accuracy of the recording.3 Internal monitoring is performed by attaching a screw-type electrode to the fetal scalp with a connection to an FHR monitor. Identify changes in the FHR recording over time, if possible. Under normal conditions, the placenta serves as a respiratory and nutritive organ. Interpretation of the FHR variability from an external tracing appears to be more reliable when a second-generation fetal monitor is used than when a first-generation monitor is used.3 Loss of variability may be uncomplicated and may be the result of fetal quiescence (rest-activity cycle or behavior state), in which case the variability usually increases spontaneously within 30 to 40 minutes.19 Uncomplicated loss of variability may also be caused by central nervous system depressants such as morphine, diazepam (Valium) and magnesium sulfate; parasympatholytic agents such as atropine and hydroxyzine (Atarax); and centrally acting adrenergic agents such as methyldopa (Aldomet), in clinical dosages.19. Cardiotocography (CTG) is the current standard of care for external monitoring of a fetus during a non-stress test (NST) and a contraction stress test (CST), as well as during labor. Retrospective studies of the NST by Platt and associates134 and of the CST by Garite and colleagues135 indicate that the use of FHR testing has been linked to a significant reduction in antepartum fetal deaths. Differentiating between a reassuring and nonreassuring fetal heart rate pattern is the essence of accurate interpretation, which is essential to guide appropriate triage decisions. Best time for a conference call or a meeting is between 4pm-6pm in GMT which corresponds to 8am-10am in PST. In: StatPearls. A cardiotocography is a technique that is used to monitor the heartbeat of the foetus along with keeping a check on uterine contractions. WebTime conversion from Greenwich Mean Time (+0) to Pacific Standard Time(-8) to EET (Eastern European Time)(+2) to Newfoundland Standard Time(-3) to Alaska Daylight Time(-8) to PDT (Pacific Daylight Time)(-7) to Central Standard Time(-6) to Eastern Standard Time(-5). Mosby: 2010. Fetal heart rate patterns are classified as reassuring, nonreassuring or ominous. bed on the whiteboard. Common examples of risk include prolonged pregnancy; maternal hypertensive disorders; intrauterine growth retardation; diabetes mellitus; Rh sensitization; maternal hemoglobinopathies; renal disease; cardiac disease; fetal anomalies; poor prior obstetric history; and reported decrease in perceived fetal movement. The incidence of reactive tests associated with subsequently negative CSTs is nearly 100%. The concept behind a non-stress test is that adequate oxygen is required for fetal activity and heart rate to be within normal ranges. This requires frequent palpation of the uterine fundus and accurate placement of the tokodynamometer. These states of active sleep occupy 4060% of the average 24-hour day18 and are also reflected by increased baseline FHR variability. The test involves attaching one belt to the mothers abdomen to measure fetal heart rate and another belt to measure contractions. If your baby doesn't move during the NST, try not to worry. Note association of accelerations with fetal movements. It is also important to remember that interpretative standards different from those used at term should be applied to these earlier gestational ages. To date, there have been four randomized controlled clinical trials of NST as a primary screening method for high risk pregnancy.128, 129, 130, 131 While most current practices would perform testing more frequently than was the case in these trials (at least twice weekly as opposed to once weekly), it is interesting to note that NSTs were generally not the only well-being tools used. Web2. Br J Obstet Gynaecol 87: 270, 1980, Vorher H: Placental insufficiency in relation to post-term pregnancy and fetal postmaturity. Why is the doctor wanting me to do a blood test, saying it might show a difference in my allergy levels. The stimulator is applied to the maternal abdomen in the region of the fetal head, then a 3-second pulse is delivered. A single copy of these materials may be reprinted for noncommercial personal use only. They are usually associated with fetal movement, vaginal examinations, uterine contractions, umbilical vein compression, fetal scalp stimulation or even external acoustic stimulation.15 The presence of accelerations is considered a reassuring sign of fetal well-being. Under adverse circumstances (e.g., decreased utero-placental perfusion or maternal malnutrition), these stores may be prematurely exhausted; consequently, fetal growth and energy-dependent biophysical activities are curtailed. In a large longitudinal study of fetuses who exhibited a combination of nonreactivity, reduced variability, and spontaneous decelerations, Beischer and associates124 found that 93% of surviving infants available for follow-up had no major neurologic handicap. Am J Obstet Gynecol 133: 685, 1979, Peeters LL, Shelton RE, Jones MD et al: Blood flow to fetal organs as a function of arterial oxygen content. Br J Obstet Gynaecol 89: 427, 1982, Kidd LC, Patel NB, Smith R: Nonstress antenatal cardiotocographya prospective randomized clinical trial. Most obstetric laboratories now use FHR transducers operating in either continuous or pulsed Doppler modes rather than phonocardiographic or abdominal electrocardiographic signal sources. Am J Obstet Gynecol 135: 1071, 1979, Nathanielsz PW, Bailey A, Poore ER et al: The relationship between myometrial activity and sleep state and breathing in fetal sheep throughout the last third of gestation. This is presumptive support of the effectiveness of the reactive test alone in identifying uncompromised fetuses. In the absence of acidosis, acute disturbances of placental respiratory or nutritive function may result in sudden and profound decrease in fetal movement incidence. WebLow risk patients with metastatic disease were, however, significantly more likely to need to change to second line chemotherapy than patients with non-metastatic GTN although Am J Obstet Gynecol 170: 650, 1994, Searle JR, Devoe LD, Phillips MC, Searle NS: Computerized analysis of resting fetal heart rate tracings. In Pecile A, Finzi C (eds): The Foeto-Placental Unit, p 323. Br J Obstet Gynaecol 84: 39, 1977, Schifrin BS, Lapidus M, Doctor GS et al: Contraction stress for antepartum fetal evaluation. Fetal tachycardia may be a sign of increased fetal stress when it persists for 10 minutes or longer, but it is usually not associated with severe fetal distress unless decreased variability or another abnormality is present.4,11,17. Labour and delivery: all you need to know, Pregnancy diet plans: trimester by trimester, Pregnancy symptoms you should never ignore, , : , : , : . It is important to maintain proper perspective on the place of FHR testing in overall clinical management. Am J Obstet Gynecol 151: 1074, 1985, Devoe LD: Antepartum fetal heart rate testing in pre-term pregnancy. Mayo Clinic on Incontinence - Mayo Clinic Press, NEW Mayo Clinic on High Blood Pressure - Mayo Clinic Press, Mayo Clinic on Hearing and Balance - Mayo Clinic Press, FREE Mayo Clinic Diet Assessment - Mayo Clinic Press, Mayo Clinic Health Letter - FREE book - Mayo Clinic Press, Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic School of Continuous Professional Development, Mayo Clinic School of Graduate Medical Education, Book: Mayo Clinic Guide to a Healthy Pregnancy. This content does not have an English version. Talk to your health care provider about your nonstress test results. This finding during the CST should prompt ultrasound examination for amniotic fluid volume, or umbilical cord localization. New York, Academic Press, 1970, Lee CY, Diloreto PC, O'Lane JM: A study of fetal heart rate acceleration patterns. GMT to Kaliningrad call time. If the results are unusual, your doctor may suggest further testing. Of the various FHR testing schemes that have been studied, two primary methods for Table 4 lists recommended emergency interventions for nonreassuring patterns.4,14 These interventions should also be considered for ominous patterns while preparations for immediate delivery are initiated. 9. You can get one of two results from an NST: Reactive: This result means that your babys heart rate went up to the expected level at least twice during the test. Those with a reactive baseline are at much lower risk for intrauterine or neonatal compromise, while those with nonreactive CSTs constitute the highest risk group within the populations studied to date.91, 92, 93, 94 It is probable that a number of false positive tests occur in the former subgroup, and, as suggested by Devoe,103 only 10% developed evidence of intrapartum fetal distress when vaginal delivery was attempted. The most significant factor that influences fetal response to VAS appears to be gestational age.